If you think you understand the scale and impact of spasticity, prepare to be surprised. In individuals with upper motor neuron damage, a phenomenon known as clasp knife spasticity can occur, causing a unique and often debilitating form of rigidity. This condition, characterized by spastic paralysis with a clasp-knife reaction, is a complex neurological disorder that requires specialized care and management.
In this article, we will deep dive into the causes and care required for clasp knife spasticity. We will explore the mechanisms behind this condition and how it differs from other forms of rigidity. By understanding clasp knife spasticity, we can develop effective strategies to improve the quality of life for individuals living with this condition.
Key Takeaways
- Clasp knife spasticity is a unique form of rigidity that occurs in individuals with upper motor neuron damage.
- It is characterized by spastic paralysis with a clasp-knife reaction.
- Understanding the underlying mechanisms of clasp knife spasticity is crucial for effective management and care.
- Clasp knife spasticity differs from other forms of rigidity, such as cogwheel rigidity.
- Specialized strategies, including physical rehabilitation, pharmacological treatments, and emerging therapies, can help alleviate symptoms and improve quality of life.
Introduction to Clasp Knife Spasticity
In this section, we will provide an introductory overview of clasp knife spasticity. Clasp knife spasticity refers to a form of muscle rigidity commonly associated with neurological conditions. It is characterized by a phenomenon known as the clasp knife reaction, which involves a sudden resistance followed by a release in muscle tone when a limb is passively moved.
Clasp knife spasticity can have significant implications for individuals affected by it. The rigid muscle tone caused by clasp knife rigidity can limit movement and impair daily functioning. It can lead to difficulties in performing basic tasks, such as walking, dressing, and eating.
Furthermore, the damage caused by clasp knife rigidity can extend beyond physical limitations. The chronic nature of clasp knife spasticity can have a detrimental impact on an individual’s emotional and psychological well-being. Coping with the challenges posed by this condition requires a multidisciplinary approach involving healthcare professionals, caregivers, and a supportive environment.
By establishing this foundation of knowledge about clasp knife spasticity, we can better understand its impact on individuals and develop appropriate care strategies. In the following sections, we will delve deeper into the signs, mechanisms, and management options for clasp knife spasticity.
Identifying the Signs of Upper Motor Neuron Damage
Clasp knife spasticity is closely associated with upper motor neuron damage. By identifying the signs and characteristics of this damage, healthcare professionals can accurately diagnose and treat clasp knife spasticity. Some key signs to look out for include:
- Hyperreflexia: Increased reflex responses, such as exaggerated knee-jerk reflexes, can be indicative of upper motor neuron damage.
- Clasp Knife Reflex: The clasp knife phenomenon is a characteristic feature of clasp knife spasticity. It refers to the resistance encountered during passive movement, which shows a sudden release akin to the folding and closing of a clasp knife.
Characteristics of Clasp Knife Phenomenon
The clasp knife phenomenon is a distinctive characteristic of clasp knife spasticity. It is observed during the examination of muscle tone and resistance to movement. When the affected limb is moved passively, there is an initial resistance followed by a sudden, involuntary release of muscle tension, resembling the opening and closing of a clasp knife. This signature movement pattern indicates upper motor neuron dysfunction and is often seen in conditions such as cerebral palsy and multiple sclerosis.
Exploring the Spinal and Cerebral Models of Spasticity
Two models help explain the underlying mechanisms of spasticity, including clasp knife spasticity: the spinal model and the cerebral model.
The spinal model suggests that spasticity arises from hyperexcitability in the spinal cord due to disrupted inhibition of the lower motor neurons. This disruption leads to increased muscle tone, exaggerated reflexes, and the clasp knife phenomenon.
The cerebral model proposes that damage to the upper motor neurons in the brain disrupts the inhibitory signals sent to the spinal cord. This imbalance results in increased excitability of the lower motor neurons, leading to the characteristic features of clasp knife spasticity.
By understanding these models and their implications for clasp knife spasticity, healthcare professionals can develop targeted strategies for the diagnosis and management of this condition.
Neuropathology of Clasp Knife Spasticity
In this section, we will explore the neuropathological basis of clasp knife spasticity, focusing on the underlying physiological mechanisms and their association with various neurological conditions. One such condition is Parkinson’s disease, which often manifests with clasp knife spasticity as a result of altered neural pathways and motor control dysfunction.
Understanding the physiology of clasp knife spasticity in Parkinson’s disease is crucial for healthcare professionals to develop targeted treatment strategies. By delving into the neuropathology of this condition, we can gain insights into the specific mechanisms that contribute to the development and progression of clasp knife spasticity.
To visualize the neural pathways involved, refer to the image below:
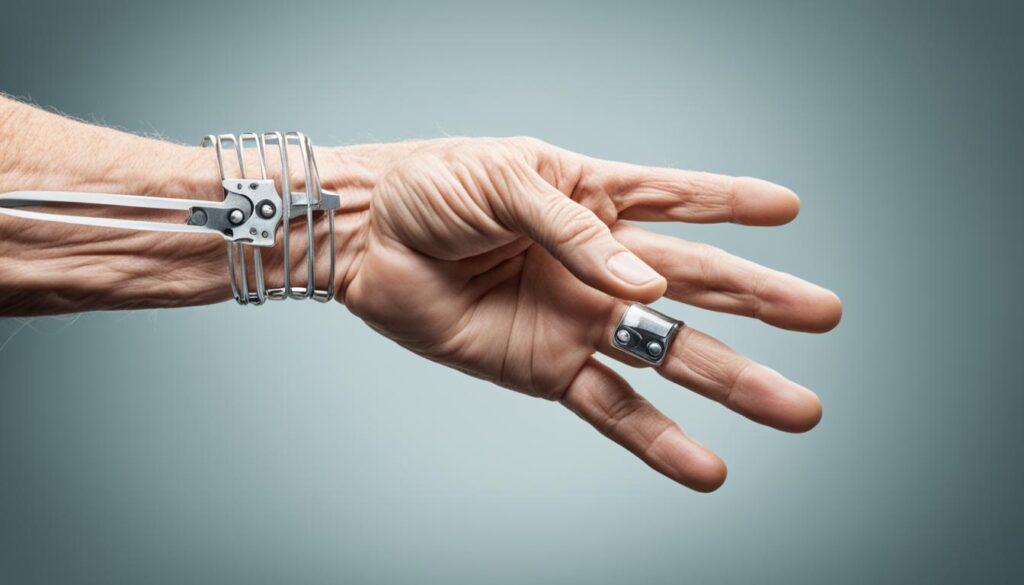
As depicted in the image, the disrupted neural connections in Parkinson’s disease result in abnormal muscle stiffness and involuntary contractions, commonly referred to as clasp knife spasticity. These motor impairments significantly impact the quality of life for individuals with Parkinson’s disease and necessitate targeted interventions to alleviate symptoms.
Overall, by unravelling the neuropathology of clasp knife spasticity, healthcare professionals can gain a deeper understanding of its underlying mechanisms, allowing for more precise treatment approaches and improved management strategies.
Neurological Conditions Associated with Clasp Knife Spasticity
| Neurological Condition | Characteristic |
|---|---|
| Parkinson’s Disease | Abnormal muscle stiffness and involuntary contractions |
| Cerebral Palsy | Impaired voluntary muscle control and coordination |
| Multiple Sclerosis | Upper motor neuron damage leading to spasticity and rigidity |
| Spinal Cord Injury | Disrupted motor pathways resulting in muscle spasticity |
Note: This table provides a brief overview of the associated neurological conditions and their characteristic features. It is important to recognize that clasp knife spasticity can occur in various other conditions and may present with nuanced symptoms.
Clasp Knife Spasticity: Delving into the Mechanism
Clasp knife spasticity is a complex condition that involves intricate neurological mechanisms. Understanding these mechanisms is crucial for effective management and treatment. Let’s explore the neurological processes and pathways underlying clasp knife spasticity, as well as the different types of spasticity associated with this condition.
Clasp knife spasticity arises from neurological damage, particularly in the upper motor neurons. It manifests as a hyperactive stretch reflex, resulting in increased muscle tone and stiffness. The mechanism behind this phenomenon can be explained by the “clasp knife” reaction, which refers to the sudden release of resistance during passive movement.
This spasticity mechanism involves an imbalance between inhibitory and excitatory signals within the central nervous system. Normally, inhibitory signals from the brain regulate muscle activity and prevent excessive contraction. However, in clasp knife spasticity, this inhibitory control is disrupted, leading to abnormal muscle tone and rigidity.
There are different types of spasticity associated with clasp knife spasticity. These include:
- Tonic spasticity: Characterized by a constant and sustained muscle contraction.
- Phasic spasticity: Characterized by intermittent muscle contractions triggered by specific stimuli.
- Rhythmic spasticity: Characterized by repetitive muscle contractions with a regular pattern.
Understanding these types of spasticity can help healthcare professionals tailor treatment approaches to address the specific manifestations experienced by individuals with clasp knife spasticity.

The image above illustrates the mechanism of clasp knife spasticity, providing a visual representation of the complex neurological processes involved.
By delving into the mechanism of clasp knife spasticity and identifying the various types of spasticity associated with this condition, healthcare professionals can develop targeted interventions and improve the lives of individuals affected by this challenging neurological condition.
Intervention Strategies for Spasticity Management
In order to effectively manage clasp knife spasticity, a comprehensive approach that combines various intervention strategies is essential. This section explores three key strategies: physical rehabilitation, pharmacological treatments including the use of botulinum toxin, and the role of surgical procedures and emerging therapies.
In addition to the comprehensive approach mentioned above, incorporating non-invasive therapies like red light therapy belts can also aid in managing clasp knife spasticity. These belts utilize red light therapy, which has been shown to promote tissue healing, reduce inflammation, and alleviate muscle stiffness. By combining red light therapy with other intervention strategies, individuals with clasp knife spasticity may experience enhanced relief and improved quality of life.
Assessing the Efficacy of Physical Rehabilitation
Physical rehabilitation plays a crucial role in the management of spasticity. Through a tailored program of exercises, stretching, and strengthening, individuals with clasp knife spasticity can experience a reduction in muscle stiffness and improved mobility. Physical therapists utilize a range of techniques such as constraint-induced movement therapy, functional electrical stimulation, and hydrotherapy to help patients regain function and enhance their quality of life. By assessing the efficacy of physical rehabilitation, healthcare professionals can optimize treatment plans and provide personalized care.
Pharmacological Treatments and Botulinum Toxin
Pharmacological treatments are another important aspect of spasticity management. Medications such as muscle relaxants, antispasmodics, and anticonvulsants may be prescribed to help reduce muscle hypertonicity and improve spasticity-related symptoms. In some cases, botulinum toxin injections can be used to selectively weaken specific muscles, effectively reducing spasticity and facilitating functional movement. This targeted approach provides temporary relief from clasp knife spasticity and can significantly improve a patient’s overall well-being.
Role of Surgical Procedures and Emerging Therapies
In cases where conservative management approaches are insufficient, surgical procedures and emerging therapies may be considered. Surgical interventions, such as selective dorsal rhizotomy or intrathecal baclofen pump implantation, target the underlying neurological causes of clasp knife spasticity. These procedures aim to decrease spasticity and improve motor control. Additionally, emerging therapies such as neurostimulation techniques, stem cell therapy, and novel pharmaceutical agents are under investigation and show promise in the future management of clasp knife spasticity. Continued research and advancements in these areas may provide new options for individuals with this condition.
Overall, by employing a combination of physical rehabilitation, pharmacological treatments, and considering surgical procedures and emerging therapies, healthcare professionals can effectively manage clasp knife spasticity and enhance the lives of those living with this condition.

Maximizing Patient Care: A Multidisciplinary Approach
In the management of clasp knife spasticity, a multidisciplinary approach is crucial to maximize patient care and enhance overall well-being. By leveraging the expertise of various healthcare professionals, including neurologists, physical therapists, and occupational therapists, a holistic treatment and support system can be established.
Collaborative efforts among different specialists enable comprehensive evaluation and tailored care plans based on the unique needs of individuals with clasp knife spasticity. This multidisciplinary approach ensures a comprehensive understanding of the condition, allowing for more informed decision-making and treatment strategies.
One key aspect of this approach is exploring various spasticity relief techniques and strategies. These techniques encompass a range of interventions aimed at reducing spasticity and improving quality of life. They may include:
- Physical therapy exercises targeting muscle relaxation and stretching
- Occupational therapy to enhance functional abilities and promote independent living
- Assistive devices and adaptive equipment to facilitate mobility and everyday activities
- Orthotics and splints to support proper positioning and reduce spasticity
- Pharmacological treatments, such as muscle relaxants or anti-spasticity medications, as directed by a healthcare professional
- Botulinum toxin injections to specifically target and weaken overactive muscles
Additionally, a multidisciplinary approach encourages collaborative discussions among healthcare professionals, enabling the sharing of knowledge, perspectives, and best practices. This collaboration fosters a comprehensive understanding of clasp knife spasticity, leading to more effective and personalized care for patients.
Overall, a multidisciplinary approach allows for a comprehensive and holistic approach to clasp knife spasticity management, maximizing patient care and improving outcomes. By adopting this approach, healthcare professionals can address the diverse needs of individuals with clasp knife spasticity and enhance their quality of life.

Conclusion
In conclusion, clasp knife spasticity is a complex condition that requires a comprehensive understanding of its causes and mechanisms in order to provide optimal care. Throughout this article, we have explored the various aspects of clasp knife spasticity, including its association with upper motor neuron damage, its unique characteristics, and the underlying neuropathology. By integrating the knowledge gained from this article, healthcare professionals can enhance their ability to diagnose, treat, and manage clasp knife spasticity effectively.
Understanding the causes of clasp knife spasticity is crucial for developing targeted intervention strategies. By identifying the signs of upper motor neuron damage and exploring the spinal and cerebral models of spasticity, healthcare professionals can accurately diagnose and treat clasp knife spasticity. Furthermore, by delving into the intricate mechanisms underlying clasp knife spasticity, we can gain insights into the specific factors contributing to this condition and develop tailored approaches for its management.
A multidisciplinary approach is key to maximizing patient care in clasp knife spasticity. Collaborative efforts between healthcare professionals, such as neurologists, physical therapists, and occupational therapists, can provide holistic treatment and support. Additionally, various spasticity relief techniques and strategies can enhance the overall well-being of individuals with clasp knife spasticity. By adopting a multidisciplinary approach and integrating these techniques, healthcare professionals can address the diverse needs of patients and improve their quality of life.
In summary, clasp knife spasticity is a challenging condition that requires a multidimensional understanding and approach. By comprehending its causes, mechanisms, and intervention strategies, healthcare professionals can make a significant impact in the lives of individuals living with clasp knife spasticity. With ongoing research and advancements in this field, the future holds promise for further improving the care and management of this condition.




